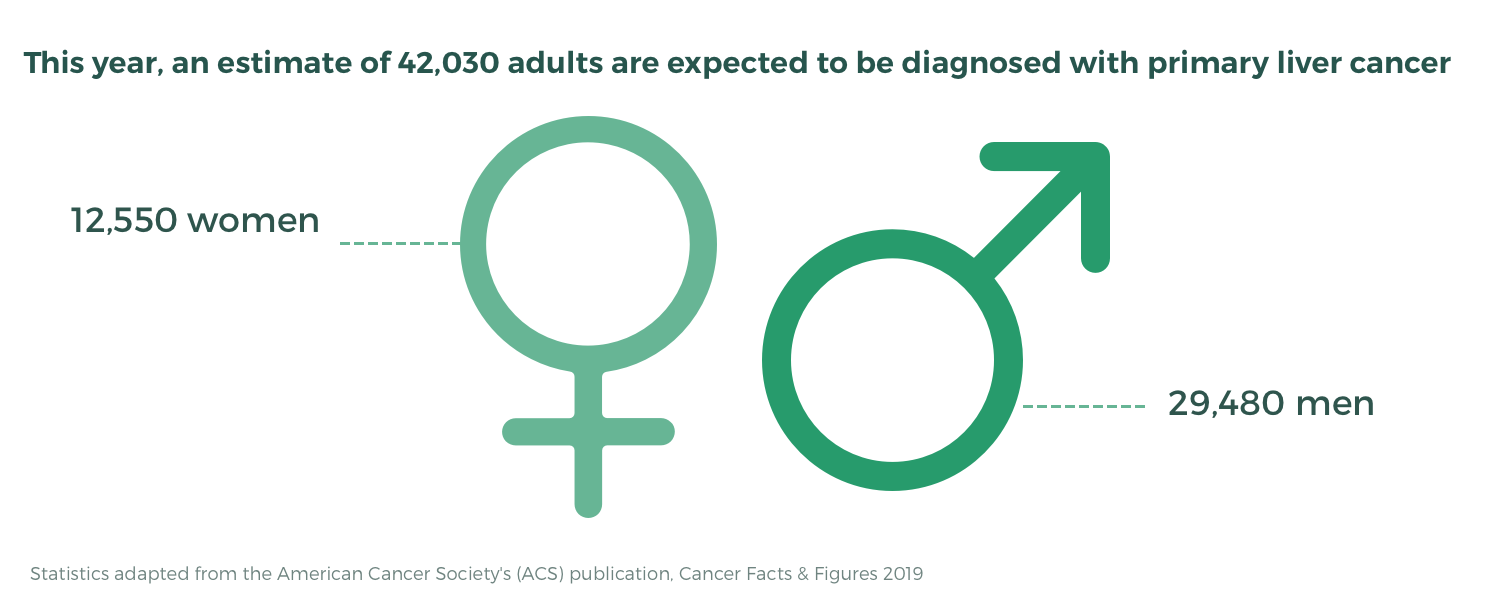
Over 42,000 American adults will face liver cancer diagnosis this year.
But accurately identifying liver lesions can be difficult, resulting in high rates of both false positives and missed diagnoses.
To help patients navigate a liver cancer diagnosis, we spoke with one of the world’s leading abdominal MRI experts, Dr. Richard Semelka. From how to ensure your liver mass was correctly identified to what questions you should ask your healthcare provider before beginning treatment, Dr. Semelka offers advice to ensure an accurate diagnosis.
DocPanel is committed to making sure every patient receives excellent care. If you would like an expert second opinion on your medical imaging scan from Dr. Semelka or one of our other abdominal subspecialists, you can learn more here.
How To Navigate a Liver Cancer Diagnosis
[DocPanel] Following a liver cancer diagnosis, what questions should patients be asking their healthcare providers?
[Dr. Semelka]
There are a few essential questions that need to be asked, beginning with:
Is it cancer or is it a benign disease, and how certain are you that it is one and not the other?
Sometimes, physicians may not be 100% sure. But they want to convey confidence, so they act as though they are. It’s a frequent problem that patients should be conscious of.
Next, a patient should ask:
Is this primary liver cancer (cancer that started in the liver)? Or, do these lesions appear to resemble and represent liver metastases (cancer that has spread from another organ)?
So, to summarize the flow of questions, the first step is to determine – Is it benign? Is it malignant? How confident are you? And if it is malignant, the next step should establish – Did it arise in the liver? Or, did it occur somewhere else and spread to the liver? Those are the immediate questions that have to be asked.
[DocPanel] What factors influence a radiologist’s, or other healthcare provider’s, ability to correctly answer the above questions? How can a patient be sure they’re getting an accurate evaluation?
[Dr. Semelka]
The most critical thing a patient needs to be conscious of is whether or not their imaging study has been interpreted by an expert. This also applies to at-risk individuals who get annual liver cancer screenings.
It is very easy for different types of liver lesions to be mistaken for one another. A lesion’s appearance also varies depending on the type and quality of the study. All these factors need to be taken into consideration by the interpreting radiologist.
For instance, if I read an outside study though DocPanel, one of the first things that I like to note in my report is whether or not the image is a good quality study. When the referring physician or patient hears that the study is of good quality – they know from the beginning that they’re in a good position to have a correct answer. Alternatively, if it’s poor quality, they know that perhaps another study should be done to eliminate the risk of something being obscured on the image.
All too often, the general public tends to assume that a radiologist automatically knows how to read an imaging study no matter what it is – be it a mammogram, a chest x-ray, or a liver MRI. People think that it’s like a blood test wherein these are the numbers and that’s just the way it is. But that’s not the case.
It takes years of experience to develop the skillset required to differentiate lesions. If your scans have been viewed by a generalist – or even if they’ve been viewed by a specialist – getting a second opinion from an expert is the best way to ensure accuracy. If the second opinion confirms the original diagnosis – you can be confident in your decision to begin treatment. And if the second opinion results in a change of diagnosis – well, that can be life-saving.
One of the major virtues and values of Docpanel is the ease at which patients can connect to real experts. It’s all online, so there’s no need to travel, and the price is a fraction of what patients would pay if they were to go to an elite hospital. When it comes to a liver cancer diagnosis, or rather any cancer diagnosis – getting a second opinion from an expert subspecialist should always be a precursor before starting treatment.
[DocPanel] What type of imaging study is the best for accurately identifying and diagnosing liver lesions?
[Dr. Semelka]
An MRI with gadolinium contrast interpreted by an expert subspecialty radiologist is typically your best bet.
But it’s important for patients to realize that it’s not about over imaging or over investigating. Not every patient will need an MRI. More important than the type of scan is the expertise of the interpreting radiologist. It takes an expert to know if and when a patient needs an MRI in the first place.
It’s also about finding someone with a great deal of knowledge that doesn’t have a conflict of interest. For instance, if I’m looking at a scan that’s sent from Germany or Ireland or wherever – there is no financial incentive for me to say oh – you need surgery to remove it.
My only interest is to use all my years of knowledge and experience to tell people what I would do if I were them. And in a complex situation, there’s no better way to convey what I truly think would be the best for a patient.
[DocPanel] What steps should be taken before beginning treatment?
[Dr. Semelka]
You really want to make sure your team of physicians is truly confident they correctly identified the type of liver lesion. Generally speaking, in the great majority of occasions, MRI of the liver will provide a definitive diagnosis. The last diagnostic tool would be a biopsy – but only when necessary.
So again, my advice would be to get a second opinion. With Docpanel you have a special opportunity for a world authority to look at your images. You want someone with as high accuracy as you can attain because, again, benign lesions are very common in the liver and an expert can recognize them better than anyone else.
You don’t want to be treated a particular way because you were told you have liver metastases when it turns out they’re actually biliary hamartomas. And at the same time, you don’t want to have a very aggressive surgical procedure if it turns out you have extensive metastases in the liver. It’s a terrible outcome, but the point being – you don’t want to spend your last days on earth very sick in the intensive care unit because you had a massive operation that didn’t even really help you in the end.
[DocPanel] Are more benign liver lesions mistaken for cancer? Or vice-versa?
[Dr. Semelka]
When I think of the errors that I correct and see people making – I’d say it’s about a 60 to 40 ratio, with more benign lesions being mistaken for malignant lesions. These can be seen as happy errors.
For instance, say a woman with breast cancer goes in for some imaging exams as part of her checkup. Now say a radiologist reviews her scans and says she has liver metastases – which, for stage 4 breast cancer, does not tend to have great outcomes. But then you have an expert review the scan and it turns out she doesn’t have metastases – she has a benign liver lesion, like hemangioma, which is really quite common and probably seen in about 10% of people. This would be a happy error, as it leaves the patient very relieved. Imagine being under the false impression that you have both breast cancer and liver metastases – the stress is huge!
[DocPanel] What risks are involved with surgical removal of liver tumors?
[Dr. Semelka]
Surgical resection is a major procedure – so the obvious biggest risk is death. But with that being said – the risk of death is quite low – at less than 1%. So it’s not something that should terrify an individual if they’re told they should get liver resection. Nonetheless, it’s important to recognize the risk. Other less serious, yet adverse, events that can occur with surgery are complications like hemorrhage and infection.
While not necessarily a risk, it should be noted that it takes quite a while for an individual to recover from liver surgery. A minor procedure can take weeks, while a major one can take months. That’s one of the reasons why many centers prefer to use local ablative therapy.
Ablative therapy uses probes or really big needles to go through the skin on the surface of the abdomen and into the liver lesion. It’s then combined usually with heat or a variation of heat – like microwave – to essentially kill the tumor and a small amount of liver around the lesion. It’s the preferred way to manage patients with multiple lesions, as seen with hepatoma and chronic liver disease/cirrhosis.
CONNECT WITH A SPECIALIST
Take Charge of Your Health
Get a second opinion from a radiology specialist in 3 easy steps.
[DocPanel] Does imaging play an important role in treatment and management?
[Dr. Semelka]
Absolutely, it’s the best way to follow the patient’s response to treatment, as well as to monitor any changes in the lesions.
During treatment, ultrasound is good for monitoring a lesion’s size. MRI is especially important, as it gives us a better sense of a lesion’s viability. In other words, it tells us how alive the lesion is. When treating multiple lesions, a gadolinium-enhanced MRI is typically the best because it’s the most capable of catching small tumors. The earlier (smaller) you can catch cancer, the better off your long term outcome will be.
Imaging is also noninvasive – meaning you’re not being poked with needles and other things that put you at risk for complications.
[DocPanel] What risks are associated with biopsy? Under what circumstances is one recommended?
[Dr. Semelka]
With vascular lesions, a biopsy can result in hemorrhage – which can lead to other complications. It can also result in infection. The biggest risk, however, is that the needle can track cancerous cells into other parts of the liver tissue when the needle is being pulled out. This doesn’t always happen – but it’s a risk.
Now, one might be thinking – well, isn’t pathology (biopsy) 100% accurate in determining malignancy? And shouldn’t that outweigh the risks? But the truth is, no. There are several things that can go wrong with a liver biopsy, bringing accuracy down to somewhere around 85%.
If I were to give approximate accuracy percentage rates for liver lesion diagnosis using expert-interpreted MRI, CT, and ultrasounds, they’d go as follows:
- MRI – 95% accuracy
- Biopsy – 85%
- CT – 80%
- Ultrasound – 65%
So while a biopsy is better than CT, it’s not better than MRI. It’s also important to realize that if you’re an expert, you should know when a biopsy is necessary and when it’s not. It’s very circumstantial.
For example, I was once treating a patient for a liver lesion who had both melanoma and chronic liver disease. Now, melanoma can spread to the liver as metastases and liver disease can develop into hepatoma. But correctly differentiating these two types of liver lesions is tricky because both appear bright on a set of images. Yet it’s crucial because treatment for one varies greatly from the other.
It is rare occasions, like this, where it’s imperative that I recognize the fact that I don’t think I can make the differentiation confidently. In these instances, a biopsy is a good idea.
A true expert does not think that everything they’re doing is always the best. A true expert knows their strengths and their weaknesses. They know the limitations of what they do, and they know when something else is needed.
While liver cancer may be on the rise, the outcome doesn’t have to be threatening. When caught early, proper treatment can turn a liver cancer diagnosis into a manageable chronic condition.